Month: November 2020
All-on-4
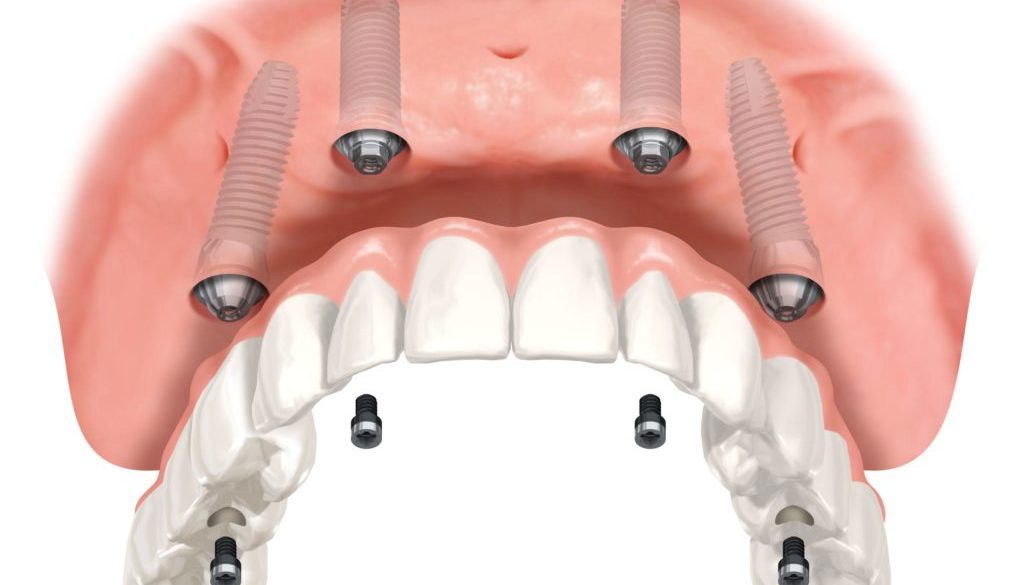
The term All-On-4 refers to “all” teeth being supported “on four” dental implants, a prosthodontics procedure for total rehabilitation of the edentulous patient or for patients with badly broken down teeth, decayed teeth or compromised teeth due to gum disease. It consists of the rehabilitation of either edentulous or dentate maxilla and/or mandible with fixed prosthesis by placing four implants in the anterior maxilla, where bone density is higher. The four implants support a fixed of surgery.
All-On-4 is not an invention, but rather a treatment technique that has evolved over time and prosthesis with 10 to 14 teeth and it is placed immediately, typically within 24 hours.
The technique evolved when in an attempt to avoid certain anatomical limitations typically seen in the back of the upper and lower jaws have, clinicians successfully avoided bone-deficient areas with the use of angulated implants. Anatomical limitations are more prevalent in patients with full dentures, and once the back implants are placed at an angle there is often only enough room left for two more implants in the front. This has led to the use of only four fixtures to support a full set of teeth.

Receding Gums
Gingival recession, also known as receding gums, is the exposure in the roots of the teeth caused by a loss of gum tissue and/or retraction of the gum margin from the crown of the teeth.

There are many possible causes for gingival recession:
- Hereditary thin, fragile or insufficient gingival tissue predisposes to gingival recession.
- Gum disease (periodontal disease). Poor oral hygiene allows bacteria to build up between the teeth and below the gumline, which leads to painless, chronic inflammation of the gums and gradual recession.
- Overaggressive brushing, which causes the enamel at the gum line to be worn away over time by scrubbing the sides of the teeth in a washboard fashion
- Excessive clenching and grinding of the teeth (bruxism) can sometimes worsen the pre-existing periodontal disease.
- Adult orthodontic movement of teeth.
- Abnormal tooth position, such as tooth crowding, giving an inadequate cover of one or more teeth by the jaw bone.
Treatment should start with addressing the problem(s) that caused the gum recession. If overactive brushing is the cause, the patient should consider purchasing a softer toothbrush and use a more gentle brushing technique. If poor plaque control was a contributing factor, improved oral hygiene must be performed, combined with regular professional dental cleanings as prophylaxis. If severe calculus (tartar) was the cause, then a procedure called scaling and root planing may be necessary to clean the teeth and heal inflammation in the gingiva (gums). If malocclusion (incorrect bite) was a factor, an occlusal adjustment (bite adjustment) or bite splint may be recommended.
Gum grafting:
Once cause-specific measures are corrected, soft-tissue graft surgery may be used to create more gingiva. The tissue used may be autologous tissue from another site in the patient’s mouth, or it can be freeze-dried tissue products or synthetic membranes.
Depending on the shape of the gum recession and the levels of bone around the teeth, areas of gum recession can be regenerated with new gum tissue using a variety of gum grafting “periodontal plastic surgery” procedures performed by a specialist in periodontics (a periodontist). These procedures are typically completed under local anesthesia with or without conscious sedation, as the patient prefers. This may involve repositioning of adjacent gum tissue to cover the recession (called a pedicle graft) or use of a free graft from the roof of the mouth (called a free gingival graft ). Alternatively, a processed donated human skin allograft may be used instead of tissue from the patient’s own palate.
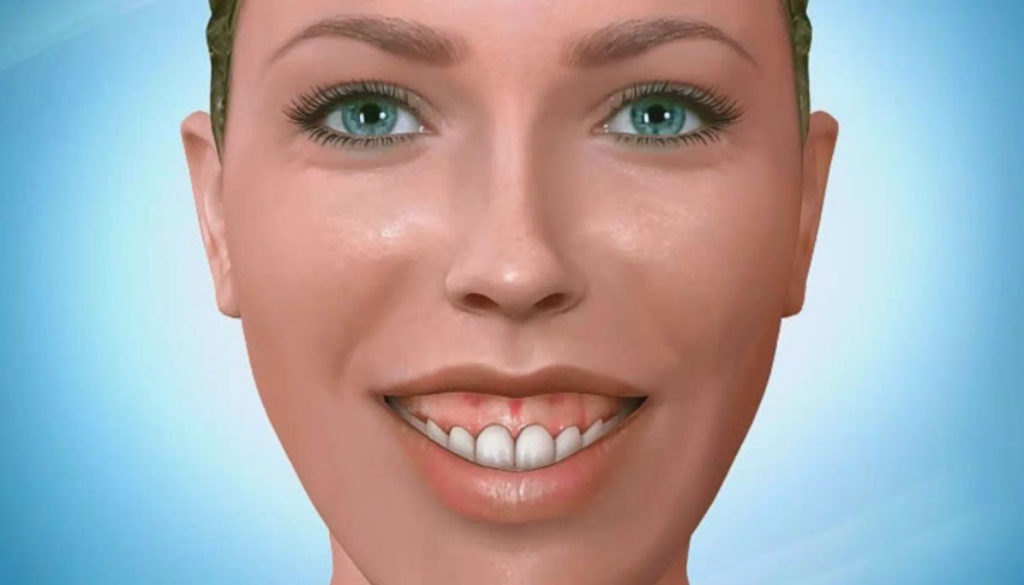
Gummy Smiles
 A gummy smile is a highly subjective diagnosis that shows tremendous variability over dental and non-dental populations. When patients identify gingival display as an area of concern, a restorative dentist has to be able to determine the etiology prior to investigating treatment options.
A gummy smile is a highly subjective diagnosis that shows tremendous variability over dental and non-dental populations. When patients identify gingival display as an area of concern, a restorative dentist has to be able to determine the etiology prior to investigating treatment options.
The gingival level is the gingiva to lip relationship. A study conducted by Dr. Vincent Kokich Jr., asked a group of lay people, orthodontists and general practitioners what they thought about acceptable gingiva levels for smiles. The results are somewhat surprising.
Lay people: Those who were not professionals viewed the threshold at 3mm; when the gums hit the 3 mm mark they rated the smile as less attractive.
Orthodontists: Orthodontists rated their threshold at 2 mm, the strictest requirement in the study group.
General practitioners: Surprisingly, the threshold for GPs was 4 mm, the most lenient of the study group. The important question is: When do we treat a gummy smile? When it bothers the patient. The ideal target is to get somewhere under 3 mm for patients who desire to change their smiles. Before treatment, it’s necessary to understand exactly what causes a gummy smile. There are at least seven different causes, and if you don’t diagnose the cause correctly, you’re going to pick the wrong treatment for your patients.
Causes of gummy smile:
- Short upper lip (if a patient has an extremely short upper lip it’s not going to cover gingiva and their upper teeth)
- Hypermobile lip (lip moves too much)
- Vertical maxillary excess VME (short ramus and overgrowth of maxilla)
- Anterior over-eruption (excess overbite)
- Wear and compensatory eruption
- Altered active eruption (the teeth don’t make it out of bone)
- Altered passive eruption (gum doesn’t recede as the person matures)
Traditional Methods for Treating a Gummy Smile:
Orthodontics: Intrudes over erupted teeth and levels them to correct position so that it eliminates gingival display.
Periodontal surgery: Crown lengthening to move gingival levels apically, typically performed on short teeth.
Orthognathic surgery: Moves the maxilla in an apical direction impacting the maxilla.
For instances when these traditional methods of treatment won’t work, such as a patient has a hypermobile lip, there are a couple of non-traditional methods:
Botox: Studies suggest Botox, when injected into the muscles of the upper lip can to be an effective method; however, the improvement is temporary and must be repeated every three to six months.
Lip repositioning surgery: Severs the muscles that elevate the lip so it can no longer rise as far in a smile. An irreversible solution diagnosis is the key to a successful outcome.
Main bnner
Header Info
Hello world!
Welcome to WordPress. This is your first post. Edit or delete it, then start writing!
